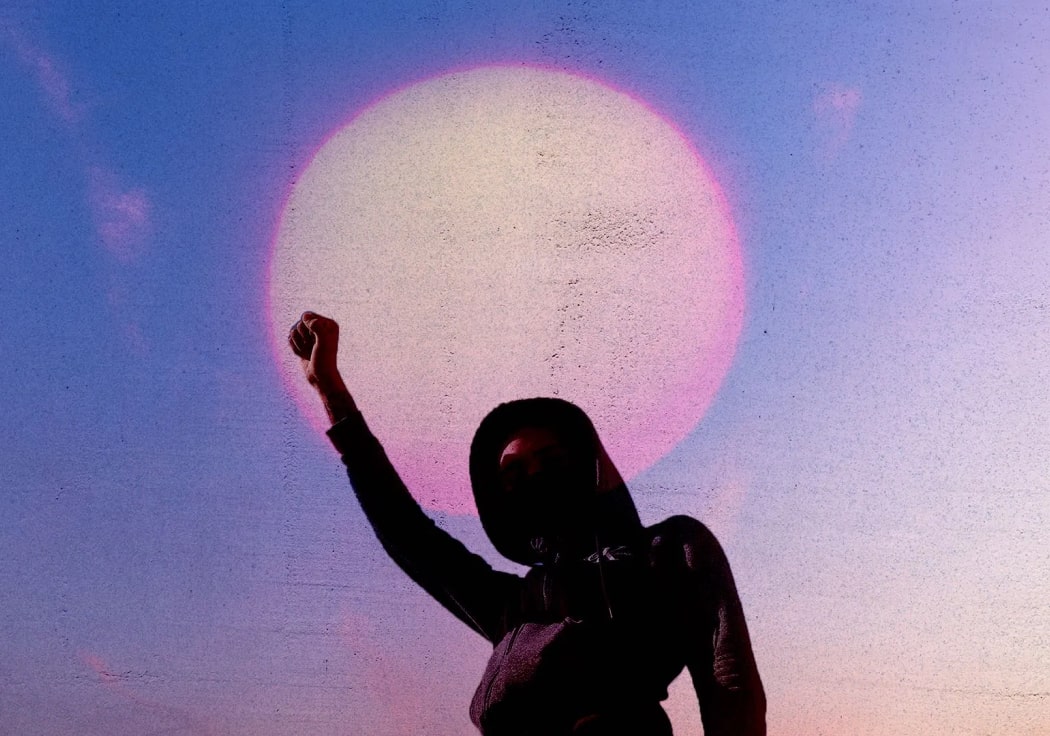
When my father first responded to the desperate NHS pleas for overseas doctors in 1992, he never expected to hear back. He was leading a happy life in a small provincial town in northern Punjab. He lived in a land nourished by five rivers, on the fault lines of the cold war that had bloodied its ancient waters. A nation where being illiterate meant you were well versed in the poetic epics of fifteenth-century sufi mystics, but signed with a thumbprint. The Royal College of Psychiatry immediately sent a job offer. He placed the letter in his bedside drawer and forgot about it. A second letter came through a few months later, a friendly reminder to respond, outlining work perks with the NHS such as accommodation on site. He placed this also in his drawer and forgot about it, until my mother found it a few months later. My father distinctly remembers becoming the second BAME consultant psychiatrist in Yorkshire, and for a long time the only BAME consultant after his Nigerian colleague retired, in a country where over two thirds of doctors in his specialty were BAME. Polite bewilderment was the modus operandi of institutional racism. No one understood his enthusiasm for addressing the mental health needs of ethnic minorities, setting up cross-cultural clinics and attempting to improve translation services – they found it all rather exhausting and amusing. Equally my mother, who was juggling caring for myself and my sister with her work, decided to embark on an MPhil specialising in barriers to accessing mental health services amongst South Asian women. She presented her work to three very bemused, very white, very liver-spotted male professors. Multiculturalism was in vogue in the 90s so she managed to secure funding easily – now it’s all about treating physical health to treat mental health. Inequality isn’t the first problem one thinks of when considering socially equitable systems like the NHS. Yet we know that women, BAME, LGBT and working class patients receive varyingly substandard care. This subtle (sometimes not so subtle) disparity in treatment is mirrored in the professional hierarchy. The first time he helped to organise post-graduate exams for psychiatric trainees, my father encountered his first conversation about institutional racism with a colleague of colour who was drafted in to replace an examiner at the last minute. Most of the trainees sitting the exams were BAME, immigrants from the commonwealth, fed and watered to creep the vines of the post-colonial bureaucracies bequeathed to them by their former masters. Their medical schools used a British curriculum, British textbooks, and encouraged British accents. Yet the examiner shared her concern that, in was her experience, white candidates had to work hard to fail while candidates of colour had to work hard to pass. My dad watched a lot of Emmerdale when he first moved to Yorkshire, to get to grips with the accent: the thick Barnsley flow, as undulating as the hills from which it sprang. Particular cultural references of the northern climes were as esoteric to him as the abundant richness of his earthy Punjabi english was to them. India was exotic – coconut sighs, lotus moons and monsoon dreams. Pakistan was Bradford riots, paki bus-drivers, curry-munchers, we’re full up, I’m sorry but we are far FAR too full. When former Pakistani cricketer Imran Khan married Jemima Goldsmith and their wedding photos splashed the cover of the Daily Mail, a nurse asked my father if “his people” had structurally-sound housing in Pakistan. He politely explained they actually lived in trees like monkeys, but it was a common enough error to make and she really shouldn’t worry about it. He left the room as she belatedly realised he was joking. Like many immigrants of their generation, my parents were relieved to receive the crumbs of acceptance swept off the table in their direction. Many senior colleagues supported him and wished to see him succeed, yet he will never forget the awkward encounters that left him frustrated and angry and unable to vocalise exactly why. Back in the 90s doctors received a four-year working visa. He was halfway through his third year when he started to apply for specialty training which would take a further three years and require a renewal of his visa. His assigned mentor, the Professor of Psychiatry, tried to encourage him to leave the country. He urged him to give up thoughts of training further, spend his remaining year and a half filling his bank account with locums before getting the next boat back to the motherland. In the face of the recruitment crisis that Psychiatry was (and still is) facing, this was at best absurd advice, and most likely very, very racist. My father insisted he wanted to train further. But what if the Home Office refused to renew his visa? My father was adamant. The post-graduate dean, who had joined the meeting, sat nervously rubbing his collar, assuring my father they would support his visa application when the time came. The stereotype that south Asian migrants want their children to become doctors is well established, some of the best (or perhaps worst?) moments on Goodness Gracious Me have played upon this cultural trope, and the angry Asian uncle-ji memes – “I want to be an actor”, “It’s pronounced doctor, beta” – evoke half-despairing, half-humorous memories of many desi childhoods. Our parents had traversed continents for this, treading a new age Silk Road with other professionals fleeing poverty, nepotism and tyrannical oppression. They who searched for greater life opportunities would nowadays be disparagingly labelled “economic migrant”. My parents sold their wedding jewellery to fund the journey, arriving with nothing but a suitcase and the cusp of their ambitions nested in me, their only child at the time, a one-year-old baby. The day I received my acceptance letter to medical school was one of the proudest days of their lives. The famous urdu poet Allama Iqbal coined the term “Khudi” in his spiritual musings. It is a difficult term to translate, shrouded in mysticism, but essentially refers to the “self”, attaining selfhood, knowledge of the self. This state of “self-knowing” is deliberately enigmatic, transcending the boundary between individual and community, between chains of generations, the past and present, and – as Iqbal purposefully alluded – Man and God. Inferiority amongst post-colonial peoples is almost a spinal reflex and decolonisation requires knowledge of the self, which has been expertly hidden behind veils of orientalist deceit. I am a young junior doctor working in a very British, very diverse health service, where migrants have brought their skills and their devoted service from every corner of the earth, in exchange for acquiring the best clinical training the world can offer. This is where my parents first found their feet and first experienced what it was to be the outsider. This is where I discovered the inverse of myself through the lens of othering, almost as removed as if I were gazing upon an exhibit separated from me by a glass case in a museum. Not quite the medical education either myself or my parents, or indeed many other immigrants, signed up for. Illustration by Miriam Sugranyes
The Immigrant Doctor: Two generations of racism and medicine

The NHS has and continues to depend on the active recruitment of overseas doctors to stay abreast, yet immigrant doctors often encounter racism and obstacles to career development within the system.